Pregnant women are offered various scans and tests in pregnancy to try to find any health conditions that could affect the baby.
The tests are said to be there to help screen for a number of conditions, and to…
… see if further testing, or additional care/treatment is needed during pregnancy or postpartum.
The tests are said to be there to inform decisions about if further tests, care or treatment is needed during pregnancy or postpartum.
Scans are not (yet) 100% accurate. It is possible to told that you or your baby have a higher chance of having a health condition, when in fact, you or they do not have the condition at all. In such cases the scan often causes stress that could well be deemed unnecessary.
It is also possible to be told that you or your baby have a lower chance of having a health condition when you or you baby do have it.
Deciding if you should go ahead with scans is a personal choice, and the NHS in the UK say that your wishes will be respected if you decide to opt out of them. Anecdotal evidence would suggest that the majority do go ahead with all that are offered, and it is unquestionable that the run up to, and experience of, these scans can be in equal parts exciting and anxiety provoking.
In my awareness of this picture, ‘scanxiety’ (as it has become known) is a topic that I cover, along with tools to soothe it, in my book, Breathing For Pregnancy, How To Find Calm Through The Four Trimesters.
If you are pregnant, and worried about scans, or what they have brought into your pregnancy relative to your emotional landscape, breathwork is an extremely useful tool.
Some, of course, adore scans. Indeed, over recent years there has been an enormous rise in ‘Souvenir Scans’ – ultrasounds done for the purpose of reassurance, or to simply have a moment of connection by seeing the baby within on the screen and getting photos of videos to keep. These have becomes extremely popular, although not without controversy.
Scans and Tests, How Many and When
In the UK, the screening tests offered during pregnancy are either ultrasound scans or blood tests, or a combination of the two.
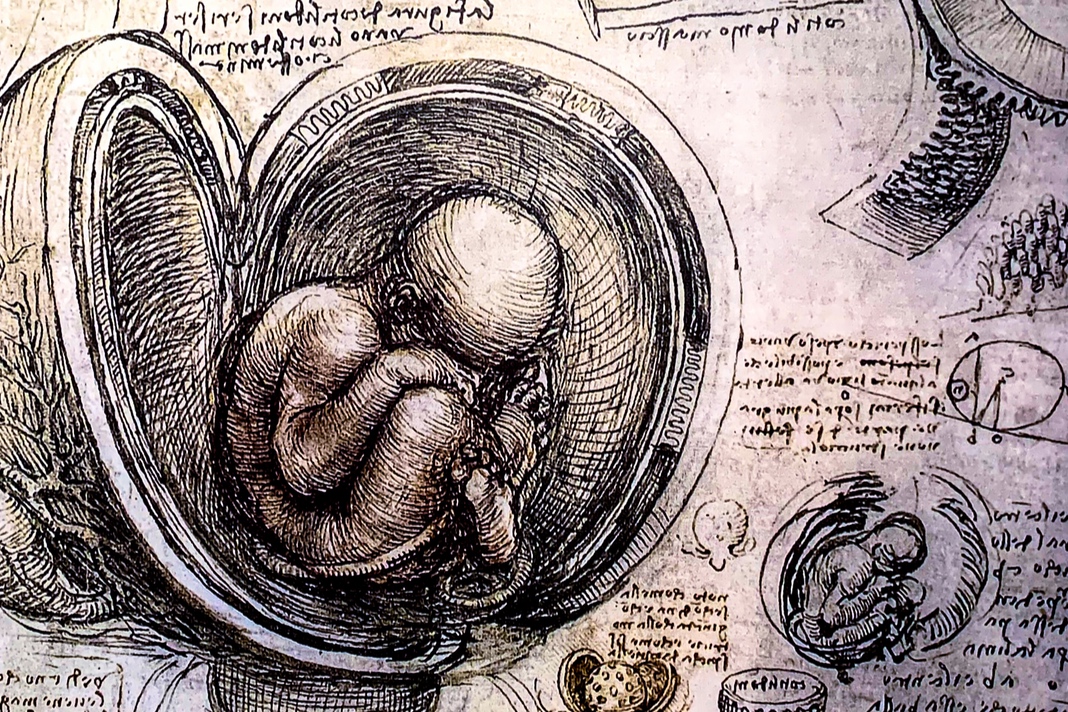
Ultrasound scans are able to (sometimes) detect conditions such as spina bifida.
Blood tests can detect an increased risk of inherited conditions, e.g. sickle cell anaemia and thalassaemia and also test pregnant women for HIV, hepatitis B and syphilis.
Blood tests combined with scans are used to give a probability of a baby having Down’s syndrome, Edwards’ syndrome or Patau’s syndrome.
The screening test for sickle cell and thalassaemia is offered before 10 weeks of pregnancy.
Screening blood tests for HIV, hepatitis B and syphilis also happen as early as possible in pregnancy. Part of what is often called ‘Booking Bloods’. Done at your first appointment with a midwife.
Screening for Down’s syndrome, Edwards’ syndrome and Patau’s syndrome are done at a dating scan, that is offered at 11 to 14 weeks pregnant.
A detailed screening to check your baby’s development – a ’20-week scan’ – is usually offered between 18 to 21 weeks of pregnancy.
Screening tests for HIV, hepatitis B and syphilis are very accurate.
Screening for Down’s syndrome, Edwards’ syndrome and Patau’s syndrome only you if your baby has a low or high chance of having the condition. Further diagnostic testing is needed, after that screening, for certainty. Such diagnostic screening comes with risks that will be outlined for individuals should it be suggested they benefit from having one.
Routine Tests You Can Expect at all Appointments
- Blood pressure check of mother: checked because raised blood pressure can be a warning sign of pre-eclampsia
- Urine tests: checked during antenatal checks for pre-eclampsia and gestational diabetes.
On top of these checks, your midwife also offers the first blood tests which look at:
- blood group and rhesus status
- infections such as hepatitis B, HIV or syphilis
- anaemia
- immunity to German measles (rubella)
- blood conditions such as sickle cell anaemia or thalassaemia.
At Around 28 weeks another blood test is sometimes done to check iron levels.
From 24 weeks, a midwife will measure your bump to check that baby is growing. Your bump is measured in centimetres from your bikini line to the top of your uterus. This is plotted on a graph.
It is considered ‘normal’ if the same as the number of weeks someone is pregnant, give or take 1–2 cm.
During the third trimester, the midwife will also do an abdominal palpation, where she feels the womb to check the position of you baby.
If you find scans, tests, hospitals and appointments hard…
You’re not alone. I know, from the huge number of pregnant women I have worked with through pregnancy, in breathwork, yoga, and as a psychotherapist, that to find these experiences something that brings worry is completely normal.
If you are particularly worried about your tests and scans it is important to speak to your doctor or midwife about how you feel.
Some charities and organisations offer support for mental health during pregnancy.
- Tommy’s: mental health before, during and after pregnancy
Call: 0800 014 7800 from Monday to Friday, 9am to 5pm, for free
Email: midwife@tommys.org - Mind: postnatal depression and perinatal mental health
Call: 0300 123 3393
Email: info@mind.org - Maternal Mental Health Alliance: COVID-19: Looking after your mental health during pregnancy and after birth
- NICE: Antenatal and postnatal mental health: clinical management and service guidance has some question ideas which might help you talk to your GP or midwife
For practices that will land you in presence, and open up a calm, reflective, space for any tests you feel a little worried about, do take a look at my book: Breathing For Pregnancy: How to find calm through the four trimesters.